Embark on a journey of discovery with our comprehensive guide to Wound Care ATI Post Test. Delve into the fascinating world of wound care, where every step brings new insights and unveils the intricacies of this essential healthcare practice.
Our exploration will navigate the principles of wound care, assessment and evaluation techniques, debridement methods, wound management strategies, infection control measures, and the crucial role of patient education. Prepare to be captivated as we unravel the secrets of effective wound management.
Wound Care Principles
Effective wound care involves adhering to fundamental principles that promote optimal healing. These principles include:
1. Maintaining a Moist Wound Environment:
A moist wound environment is crucial for promoting healing. It facilitates cellular migration, angiogenesis, and collagen synthesis. Dressings that create a moist environment, such as hydrocolloids, hydrogels, and alginates, are commonly used to achieve this.
- Hydrocolloids:These dressings absorb wound exudate and form a gel-like substance that maintains a moist environment.
- Hydrogels:Composed of water-based gels, these dressings provide a moist environment and can absorb large amounts of exudate.
- Alginates:Derived from seaweed, alginate dressings absorb exudate and create a gel that promotes wound healing.
Assessment and Evaluation
Wound assessment is a crucial step in wound care, providing essential information for determining the appropriate treatment plan. It involves a thorough examination of the wound to identify its characteristics, extent, and underlying causes.
Steps Involved in Wound Assessment
1.
-
-*Gather patient history
Review the patient’s medical history, current medications, and any recent injuries or surgeries that may have contributed to the wound.
- 2.
- 3.
- 4.
- 5.
-*Inspect the wound
Observe the wound’s size, shape, location, and depth. Note the presence of any drainage, odor, or surrounding inflammation.
-*Palpate the wound
Gently touch the wound to assess its temperature, moisture, and pain level. Determine if there is any induration or crepitus.
-*Probe the wound
Use a sterile probe to gently explore the wound’s depth and extent. This helps identify any underlying structures that may be affected.
-*Culture the wound
Collect a sample of wound drainage or tissue for laboratory analysis to identify any infectious organisms.
Types of Wounds and Their Characteristics
Various types of wounds have distinct characteristics that influence their treatment approach:
-
-*Acute wounds
Wound care ATI post-test can be a breeze with the right preparation. However, if you’re feeling a bit rusty on the physics concepts, I highly recommend checking out this physics 1 exam 1 review . It’s a comprehensive resource that will help you brush up on the basics and ace your exam.
After you’ve mastered the physics concepts, come back to wound care ATI post-test feeling confident and ready to conquer it.
These are typically clean, closed wounds that occur suddenly, such as surgical incisions or lacerations. They usually heal quickly with minimal complications.
-*Chronic wounds
These are wounds that fail to heal within a reasonable time frame, often due to underlying medical conditions or poor wound care. They may exhibit characteristics such as delayed healing, persistent drainage, and tissue necrosis.
-*Pressure ulcers
These wounds occur when pressure is applied to a specific area of the body for an extended period, leading to tissue damage. They are commonly found in individuals with limited mobility or those confined to bed or wheelchairs.
-*Diabetic foot ulcers
These wounds occur in individuals with diabetes due to impaired circulation and nerve damage. They can be difficult to heal and may lead to serious complications if not treated promptly.
Wound Assessment Tools
Several tools can assist in wound assessment, including:
-
-*Wound measurement devices
These devices help measure the size and depth of wounds.
-*Photography
Taking photographs of wounds can provide a visual record of their progress over time.
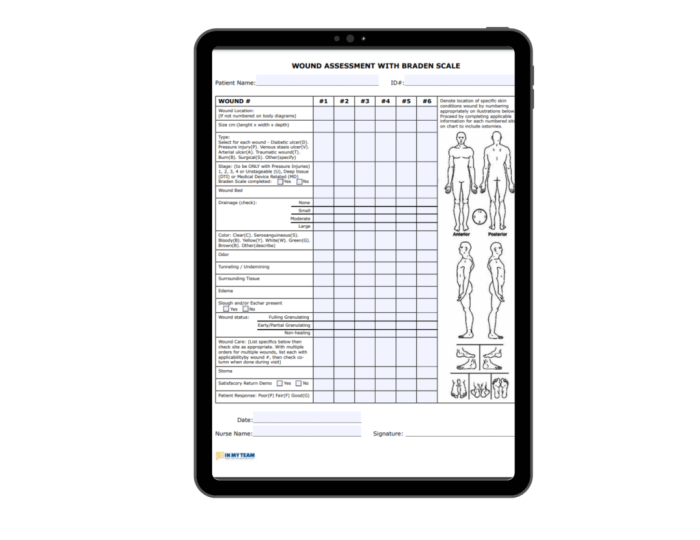
-*Wound assessment scales
Standardized scales, such as the Braden Scale for Pressure Ulcer Risk Assessment, can help evaluate the risk of developing wounds or the severity of existing ones.
Wound Debridement
Wound debridement involves the removal of non-viable tissue, foreign bodies, and debris from a wound to promote healing. It can be performed using various methods, each with its own indications and techniques.
Surgical Debridement
Surgical debridement is performed using a scalpel or scissors to remove necrotic tissue, slough, and foreign bodies. It is indicated in wounds with extensive tissue damage, infection, or the presence of foreign bodies.
Autolytic Debridement, Wound care ati post test
Autolytic debridement occurs naturally through the action of the body’s enzymes and fluids. It is indicated in wounds with minimal necrosis and a moist wound environment. Dressings that promote moisture retention can be used to facilitate autolytic debridement.
Mechanical Debridement
Mechanical debridement involves the use of physical force to remove non-viable tissue. Techniques include irrigation with a pulsatile lavage device, wound irrigation with a syringe, or the use of a wound vacuum-assisted closure (VAC) system.
Biological Debridement
Biological debridement utilizes enzymes or maggots to remove necrotic tissue. It is indicated in wounds with extensive necrosis or infection that is difficult to treat with other methods.
Chemical Debridement
Chemical debridement uses chemical agents to dissolve or loosen necrotic tissue. It is indicated in wounds with thick eschar or fibrinous exudate. Common agents include enzymatic debriding agents and hypochlorite solutions.
Ultrasonic Debridement
Ultrasonic debridement uses high-frequency sound waves to remove necrotic tissue and promote wound healing. It is indicated in wounds with biofilm or difficult-to-remove necrotic tissue.
Wound Management
Wound management encompasses various strategies to promote healing and prevent complications. This includes selecting appropriate wound dressings, implementing effective irrigation and drainage techniques, and adhering to specific protocols based on wound type.
Wound Dressings
Wound dressings serve several purposes, including protecting the wound from external contaminants, absorbing exudate, and creating a moist environment conducive to healing. Different types of dressings are used depending on the wound characteristics and stage of healing.
- Hydrocolloid dressings:Form a gel-like substance that absorbs exudate and maintains a moist wound environment, promoting autolytic debridement.
- Alginate dressings:Made from seaweed fibers, these dressings absorb large amounts of exudate and create a moist wound bed.
- Foam dressings:Provide cushioning and absorb exudate, protecting the wound from pressure and friction.
- Transparent film dressings:Allow visualization of the wound and protect it from external contaminants while maintaining a moist environment.
- Negative pressure wound therapy (NPWT):Uses a vacuum to remove exudate and promote wound healing.
Wound Irrigation and Drainage
Wound irrigation and drainage are crucial for removing debris, bacteria, and excess exudate from the wound bed. Irrigation can be performed using sterile saline or antiseptic solutions, while drainage is facilitated through the use of drains or dressings that allow exudate to escape.
Wound Care Protocols
Specific wound care protocols are established based on the type and severity of the wound. These protocols Artikel the frequency of dressing changes, irrigation, and other interventions necessary to promote healing and prevent complications.
- Superficial wounds:Typically require minimal care, with regular cleansing and dressing changes.
- Deep wounds:May require surgical intervention, antibiotics, and specialized dressings to prevent infection and promote healing.
- Chronic wounds:Often require specialized treatments such as debridement, negative pressure wound therapy, and antibiotics to address underlying factors impeding healing.
Infection Control
Wound infection is a serious complication that can delay healing and lead to other health problems. It is important to be able to recognize the signs and symptoms of wound infection so that you can get treatment as soon as possible.
The most common signs and symptoms of wound infection include:
- Increased pain, redness, or swelling around the wound
- Pus or drainage from the wound
- Fever
- Chills
- Nausea and vomiting
If you experience any of these symptoms, it is important to see a doctor right away.
There are a number of things you can do to prevent wound infection, including:
- Keep the wound clean and dry.
- Change the dressing on the wound regularly.
- Avoid touching the wound with your hands.
- Take antibiotics as prescribed by your doctor.
By following these simple steps, you can help to prevent wound infection and promote healing.
Infection Control Measures
There are a number of infection control measures that can be taken to prevent the spread of infection in a healthcare setting. These measures include:
- Hand hygiene: Healthcare workers should wash their hands frequently with soap and water or use an alcohol-based hand sanitizer.
- Personal protective equipment: Healthcare workers should wear gloves, gowns, and masks when they are in contact with patients who have infections.
- Environmental cleaning: Healthcare facilities should be cleaned and disinfected regularly to prevent the spread of infection.
- Isolation: Patients with infections should be isolated from other patients to prevent the spread of infection.
By following these infection control measures, healthcare workers can help to prevent the spread of infection and protect patients.
Patient Education: Wound Care Ati Post Test

Patient education is crucial in wound care, empowering patients to actively participate in their healing process and promote optimal outcomes. Educating patients enhances their understanding of their wound, its management, and potential complications.
Effective patient education involves various methods, including verbal instructions, written materials, and demonstrations. Healthcare professionals should tailor the education to the patient’s individual needs, considering their literacy level, language barriers, and learning style.
Written Materials
Written materials provide patients with a tangible resource to refer to after their appointment. They can include:
- Wound care instructions:Detailed instructions on wound cleaning, dressing changes, and monitoring for signs of infection.
- Educational brochures:Informative materials on wound types, healing stages, and common complications.
- Patient diaries:Trackers for patients to record wound observations, pain levels, and any concerns.
FAQ Section
What is the significance of maintaining a moist wound environment?
A moist wound environment promotes faster healing by facilitating cell migration, oxygen delivery, and nutrient exchange.
How do I assess the depth of a wound?
Use a sterile probe or cotton-tipped applicator to gently explore the wound and determine its depth.
What are the different types of wound dressings?
Wound dressings vary in material, purpose, and absorbency. Common types include hydrocolloids, alginates, foams, and transparent films.